EVERETT, Wash. – Hundreds were ill and six had died in China when a 35-year-old man touched down in Seattle after a three-month trip to visit family in Wuhan. He got sick the next day, a Thursday, saw a doctor Sunday and was admitted to the hospital Monday.
He traveled alone. He lived alone. He went into isolation. Alone.
At Providence Regional Medical Center, he spoke to doctors on the other side of the glass window through a telehealth robot and asked for a phone to call family.
It was Jan. 20, 2020, and the United States' first known case of the novel coronavirus had been reported in Snohomish County, an area of fewer than a million residents north of Seattle, flanked by the Puget Sound on the west and the Cascade Mountains on the east.
"There had to be the first case somewhere," Washington state epidemiologist Dr. Scott Lindquist told reporters crowded into a room the next day. "It was in Snohomish."
In the year since, COVID-19 has crept into every county in the nation, killing nearly 400,000 people, and infecting 1 in every 14 Americans.
While COVID-19 likely began spreading undetected elsewhere in the country, the area was the first thrust into the national spotlight – and the unknown. Along with the first official case, the region saw the first U.S. death reported at the time, the first major outbreak at a long-term care facility and the first lockdowns.
A year on, with hospitalizations nationwide at all-time highs and vaccines trudging out, residents, leaders, and medical and public health professionals looked back on those first frightening, disorienting weeks, and how they've been holding on since.
'Things are not right'
Crisis struck last year over Martin Luther King Day weekend, and many county health care staff were off work. Katie Curtis, prevention services director at Snohomish Health District, was manning the after-hours phone line that Sunday when a local clinic called to report a man with flu-like symptoms and a history of travel to Wuhan.
"I'd been hearing a bit about this virus that was happening over in Asia, never thinking that it would come here," Curtis said.
It wasn't yet clear if the patient – who has not made his identity public – had the coronavirus. Nasal swabs taken at the clinic were in transit to the Centers for Disease Control and Prevention in Atlanta. But health district staff weren't taking any chances, and Curtis was tasked with the first of a now mundane practice: contactless delivery.
On Monday, she pulled up outside the patient's home and dropped off a thermometer, some paper face masks and other supplies. She knocked on the door and left. "This was right before" it was confirmed, she said. "We were thinking, there’s something going on, things are not right."

At 7 p.m. that day, Dr. George Diaz, an infectious diseases specialist at Providence Regional Medical Center, received the news of a positive test. He'd just returned home to his wife and five kids from an infectious diseases conference in Florida, where they'd been theorizing about a potential coronavirus outbreak in the U.S. Now, the first case was on his doorstep.
Three hours later, staff maneuvered the patient into the hospital's special pathogens unit as he lay on his back in an isopod, a gurney enclosed in plastic to transport infectious patients. The staff knew what to do. They had rehearsed every move weeks before in a practice drill for an Ebola patient.
"He was pretty anxious when he arrived," Diaz said about the patient. "He had seen what was happening in Wuhan and the deaths over there."
The patient got worse before he got better. He developed a cough, fever, fatigue, diarrhea. Six days later, he developed pneumonia, and Diaz received approval from the Food and Drug Administration to administer remdesivir, an antiviral drug developed to treat Ebola. He was the first in the nation to do so.
"They’d already done the safety studies, so we knew that the drug was safe based on healthy volunteers years ago. We could tell that to the patient and that it was a good chance it would help him," Diaz said.
By Feb. 3, the patient was free.
"I am at home and continuing to get better," the man said in a statement at the time, asking for privacy. "I look forward to returning to my normal life."
Meanwhile, 20 miles south of the hospital, at Life Care Center of Kirkland in neighboring King County, the world was about to turn upside down.
'We were not equipped'
Shrouded in pine trees on a residential hilltop, the parking lot of Life Care Center of Kirkland has become a testing site months after its deadly coronavirus outbreak. Sun shines through the branches into the large bay windows of the nursing and rehabilitation center, where residents sit, looking out as staff in face shields and gloves hand plastic bags to people in their cars.
Staff pass through the front entrance, where there's a plaque dedicated to those who lost their battle with COVID-19: "Our family is broken because of your loss, but stronger because of your memory."
Nancy Butner, vice president of Life Care's Northwest Division, often finds herself walking the halls, stopping to look into the empty rooms of residents she lost to COVID-19 – the artist who taught other residents to paint, the one who always gave her packets of gum.
"Before we knew COVID, we knew of COVID," she said. When Snohomish County confirmed the first case, an unusually high number of Butner's residents were reporting flu-like symptoms. But she couldn’t get a hold of a coronavirus test until Feb. 28.
Just before midnight that evening, she got the call: Her resident had COVID-19. By 1 a.m., she and a group of staff had gathered to assess the situation, realizing just how many staff had called out sick and how many residents were potential cases.
"We had a couple boxes of N95s. We had a handful of face shields. We had plenty of surgical masks and some gowns," she said. "But we were not equipped."
The next week was the hardest of Butner’s life. Residents she'd known for almost two decades began to fall ill. In seven days, the facility sent 37 residents to the hospital, and nine died. Of 160 staff members, almost half called out sick. By the time Butner was able to secure testing for all 121 residents the following week, 101 were positive for COVID-19.
"It's like the world stopped and everyone was looking at Kirkland," Butner said. She remembers being "worried about going into the facility and learning about the loss – how many had gone out or passed that night."
It's like the world stopped and everyone was looking at Kirkland.
Butner and the staff still standing worked seven days a week for three weeks. She reused face masks and gloves and bought oversized T-shirts from Walmart to use as gowns. The phone never stopped ringing. Butner didn't have enough staff to take the calls.
"We had all these kinds of crazy calls, (we) got threats," she said. Staff members wearing Kirkland badges were asked to leave stores and their husbands and wives were told they couldn't go to work.
The "COVID-19 days" ended for Kirkland on March 30, Butner said. But it wasn't until May that the facility was able to do baseline testing of all staff, and months more before they finally obtained point-of-care testing.
At the end of August, the Kirkland community held a virtual ceremony to dedicate the memorial plaque. They lit 39 candles, one for each of the residents they lost.
What was the end of an outbreak for Life Care Center of Kirkland was just the beginning of the surge for Providence Medical Center.
'Hope and despair and frustration'
Dr. Sean Weaver saw the writing on the wall in early March. The emergency room doctor was starting a shift when he sat down at one of the nurse's stations and looked up at the board where staff record patients' chief daily complaints. More than two-thirds were having respiratory problems.
"Wuhan shut down. They built a hospital out of scratch within a couple days. Just looking at that, you knew that this was a big deal and had the potential to turn into something," Weaver said last week. "And we realized – our waiting room was filling up – was this the surge that we thought may be coming?"
As the pandemic began to take shape, Weaver had a choice to make: His wife, Rebecca, had been diagnosed with breast cancer days before his hospital admitted the first case. He was afraid of exposing her to COVID-19 and torn between his duty to family and to his patients and colleagues.
In early March, Weaver moved out into a friend's basement 20 minutes from home, leaving Rebecca to endure chemo, alone, with their two daughters, 3 and 6.
Within weeks, Weaver was working eight hours at a time without food or drink. He stood in a face mask, shield, gloves and gown at the bedside of a 70-year-old patient struggling to breathe. She had lost her husband of 50 years to COVID-19 that morning, and now she was clinging to life.
"She was there by herself in a room, grieving the loss of her partner and confidant, and I couldn’t be there with her – not in the way that I’m used to being there, and you’re not supposed to spend more than 15 minutes in the room. And so, you support as best you can," Weaver said.
That patient recovered and went home to her family a week later. But cases continued to surge at Providence through late March into early April, reaching a lull in the summer. By fall, cases were rising again, hitting an all-time high after Christmas. That's when a woman in her 60s came in complaining of shortness of breath. She quickly took a turn for the worse.
"I was going in to reevaluate her, and her heart stopped," Weaver said.
More than a dozen people rushed into the room, wanting to help but potentially exposing themselves. For more than half an hour, he tried to resuscitate the patient.
"I realized after the fact, like, I’m trying to save this woman and give her a chance of recovery, but at the same time exposing all these health care workers to this," he said. "It’s a hard thing to process."
Weaver lost the patient. He walked out of the room and sat with her husband and, later, her children.
My feelings vacillate between hope and despair and frustration. It’s odd that both can simultaneously exist.
"My feelings vacillate between hope and despair and frustration. It’s odd that both can simultaneously exist," said Weaver, who is now back home with his family. His wife is cancer-free.
"I’m hopeful with the vaccine and hopeful that there will be enough people who believe in science and that we’re going to find a way to get through this, but I also see what’s happening in Los Angeles and have a lot of sadness."
Weaver received his second dose of vaccine last week. As he waited to be monitored, he looked up at a livestream of Hollywood Boulevard and saw ambulances waiting in line for 10 hours to get into emergency departments. He spotted people walking the streets without face masks.
"It’s just ... we’ve gone through so much this past year," he said, sighing, his hands in the pockets of his white lab coat, on the sidewalk outside Providence. "We need to understand that, these last few months, before we get vaccines in people, could get very, very hard."
'Nobody turned the chapter'
For Elizabeth Baty, the month of December was the hardest one yet.
Baty, a funeral director at Flintoft's Funeral Home in King County, worked with several residents of the Life Care Center of Kirkland before they died. She had been busy all year, but her workload increased significantly last month.
"Now that we’re a year down, some people are mad. They’re mad that they’re still in this situation. They’re mad that they have to consider their own death," Baty said as she stood in Kirkland Cemetery, down the road from the nursing home.
The pandemic has lasted so long now that friends and families who opted for cremation services last spring and delayed funerals – hoping they'd be able to gather and mourn properly by summertime – are now calling her back, asking to arrange small or virtual services.
"Nobody turned the chapter, it’s just left unresolved grief – that sadness," she said. "For the spouses, especially, they feel like they never finished, like the person's still at the nursing home, sequestered somewhere else they can’t go visit."
Nobody turned the chapter, it’s just left unresolved grief – that sadness.
Over the past year, Baty has helped dozens of people in nursing homes make pre-arrangements by passing clipboards of paperwork over chain-link fences to nurses or social workers. Every so often, she's notified that it's time to put the arrangements into place – that another human life has slipped away in silence.
About half an hour north, at a cemetery on the Tulalip Reservation, Teri Gobin watches through a fence as gravediggers bury a young woman who died of COVID-19. Dozens of tribal members gather to beat hand drums outside the cemetery overlooking the sound.
"Everybody knew her out on the water. She was a crabber," Gobin said.
Gobin, chairwoman of the Tulalip Tribes – about 5,000 fishing peoples descended from the Snohomish Tribe – knows her community has weeks of collective mourning ahead of them, once the pandemic has ended.
"Our tradition is to be with the family for three to five days, bringing food, comforting, singing and showing respect. So it’s been really, really tough not to be there for each other," she said. "They will each get a day to have a memorial service. But that’s going to be a lot of time with memorial services."
Like many Native American communities, the Tulalip Tribes have been hit hard by the pandemic. Hundreds have had the virus and 60 members have died in the past year from COVID-19, opioid overdoses and other causes, Gobin said.
"It just doesn’t stop. It’s a trying time, and our people are just hurting," Gobin said. "But I’ve always been an optimistic person, and I always look to the future. I try to bring that ray of hope to our people, telling them we’ll get through."
The vaccine, Gobin hopes, will be their lifeline.
'We're going to make it'
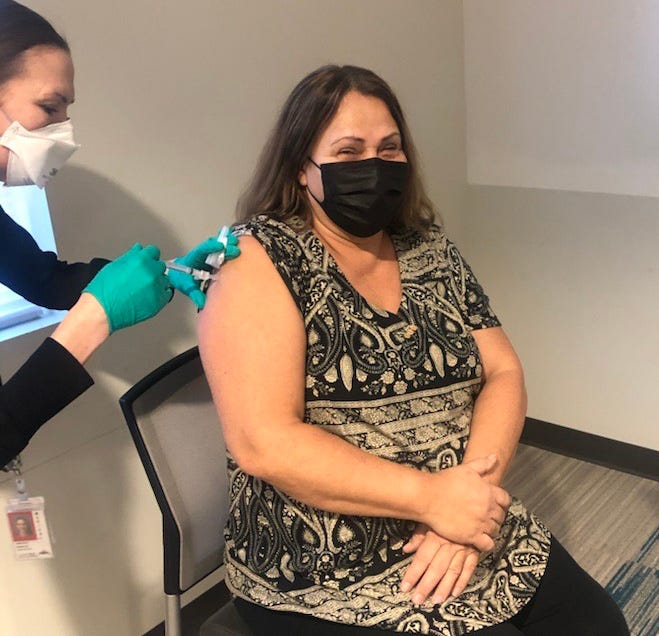
The first doses of vaccine arrived in Snohomish and King counties on Dec. 17. The rollout has been slow but encouraging.
"It was just like, oh my gosh, we can finally see we’re going to make it. We’re going to get there," said Curtis, the Snohomish Health District official. "We're all kind of energized by that."
Nearly 100,000 residents have tested positive in the two counties over the past year, and more than 1,500 people have died. In the past month, nearly 2% of Snohomish County residents and nearly 4% of King County residents have received a first vaccine dose.
At Life Care Center of Kirkland, vaccines began rolling out Dec. 28. "We took a lot of pictures and had a good celebration," Butner said, laughing. The facility has vaccinated 95% of residents and 90% of staff.
At the Tulalip Reservation on Jan. 13, a long line of more than 100 people snaked out of the community vaccination center and down to Tulalip Bay. A windstorm the night before had knocked out power across the county, starting the clock on the hundreds of Moderna vaccines in the tribe's freezer that had begun to thaw.
The clinic staff contacted Gobin that morning in a panic, and she put out an emergency call to rally people to the site. Community members flocked down to the building: tribal elders, local teachers, Snohomish County first responders.
Not a single dose went to waste.
It takes a whole lot of prayer from the whole community to get through this. We’ll get through it together.
A community that had been vaccinating 150 people a day gave out 700 in a matter of hours.
"It takes a whole lot of prayer from the whole community to get through this," Gobin said, nearly a year to the day the first patient touched down in Seattle. "We’ll get through it together."
What was the past year like for a COVID-19 patient in Snohomish County? Stay tuned for an in-depth feature.
Follow breaking news reporter Grace Hauck on Twitter at @grace_hauck. Follow multimedia journalist Harrison Hill on Twitter at @HarrisonHill.