With the current opioid crisis in the US, finding new non-addictive painkillers and other relief methods is key. An experimental, non-opioid drug known as EMA401 is showing promise, and now researchers at Washington University in St Louis have found that it works by targeting a different part of the body, outside of the nervous system.
After about 64,000 opioid-overdose deaths in 2016, the Department of Health and Human Services declared a public health emergency, and a key part of dealing with the issue is the development of new treatments and drugs. Some of these include snail venom, green light, ultrasound-triggered nerve blockers, and even marijuana, while other teams are experimenting with exploiting the brain's natural pain relief methods, blocking the pathways that lead to addiction, or disrupting pain-signaling proteins.
Recently, the experimental drug EMA401 has been shown to be an effective painkiller, particularly for lingering pain after a bout of shingles. While studying how it works, the Washington researchers discovered that unlike almost all other pain treatments, EMA401 doesn't target nerve cells.
"We are in dire need of good pain-killing drugs, particularly non-opioid drugs," says D.P. Mohapatra, principal investigator on the study. "Generally, scientists have the understanding that targets for treating pain must be within the nervous system. It turns out that the target here is not on nerve cells, but on immune cells called macrophages."
Like many drugs designed to lower blood pressure, EMA401 inhibits the angiotensin II type 2 receptor. Interestingly though, it affects those receptors on macrophages, not nerve cells. This mechanism could open up a whole new way to treat pain, without the risk of addiction or the other negative side effects of opioids.
"The beauty of this drug is that, unlike an opioid, it doesn't cross the blood-brain barrier, so right away you eliminate a number of potentially harmful side effects, including addiction and the potential for abuse," says Mohapatra. "And by widening the scope of potential targets to macrophages, it may be possible to develop more effective therapies for chronic, neuropathic pain."
The researchers made the discovery in tests on cultured mouse cells. Angiotensin is a hormone that constricts blood vessels and can cause pain, but when the team added it to a dish of nerve cells, no pain signals were transmitted.
"We found that the receptor the drug affected wasn't on the nerve cells; it was on macrophages, the immune cells," says Andrew Shepherd, co-investigator on the study. "When we added macrophages to the dish alongside the nerve cells, the angiotensin could 'talk' to the macrophages, and then the macrophages 'talked' to the nerve cells, which then transmitted pain signals."
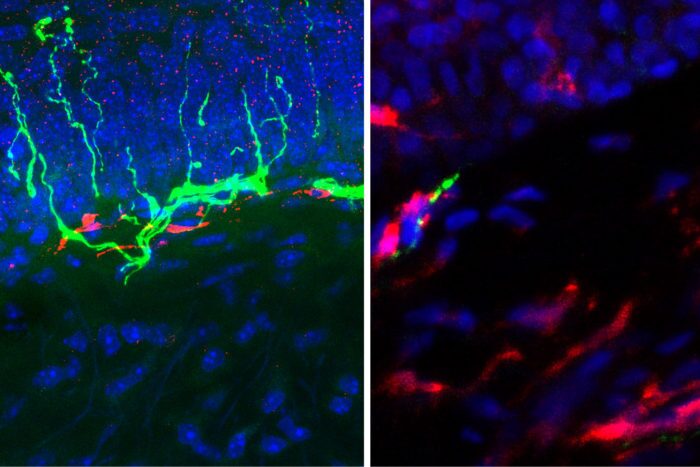
The researchers then focused on this new pain relief target. They found that live mice injected with angiotensin showed no signs of pain after the scientists reduced the number of macrophages in the animals. Normal pain responses returned after a few days, when the macrophages recovered.
The team also found much higher numbers of macrophages in people with chronic leg pain induced by diabetes, which backs up the idea that these cells are a great potential new target for pain relief drugs.
The research was published in the Journal of Neuroscience.