 Dental implants are made of commercially pure titanium or titanium alloy and are generally quite strong. However, they can fracture if placed under excessive load. Dental implant fractures occur mainly from excessive amounts of lateral force. This can be a result of an implant restoration that has not been properly equilibrated or one with significant cantilever and off-axis forces. Dental implants may also fracture if the diameter of the implant is too small for the its supporting restoration. For example, a 4-mm diameter implant for a molar may have higher risk of either implant or abutment-screw fracture due to excessive cantilever forces on the restoration.
Dental implants are made of commercially pure titanium or titanium alloy and are generally quite strong. However, they can fracture if placed under excessive load. Dental implant fractures occur mainly from excessive amounts of lateral force. This can be a result of an implant restoration that has not been properly equilibrated or one with significant cantilever and off-axis forces. Dental implants may also fracture if the diameter of the implant is too small for the its supporting restoration. For example, a 4-mm diameter implant for a molar may have higher risk of either implant or abutment-screw fracture due to excessive cantilever forces on the restoration.
There are three treatment options for fractured dental implants:
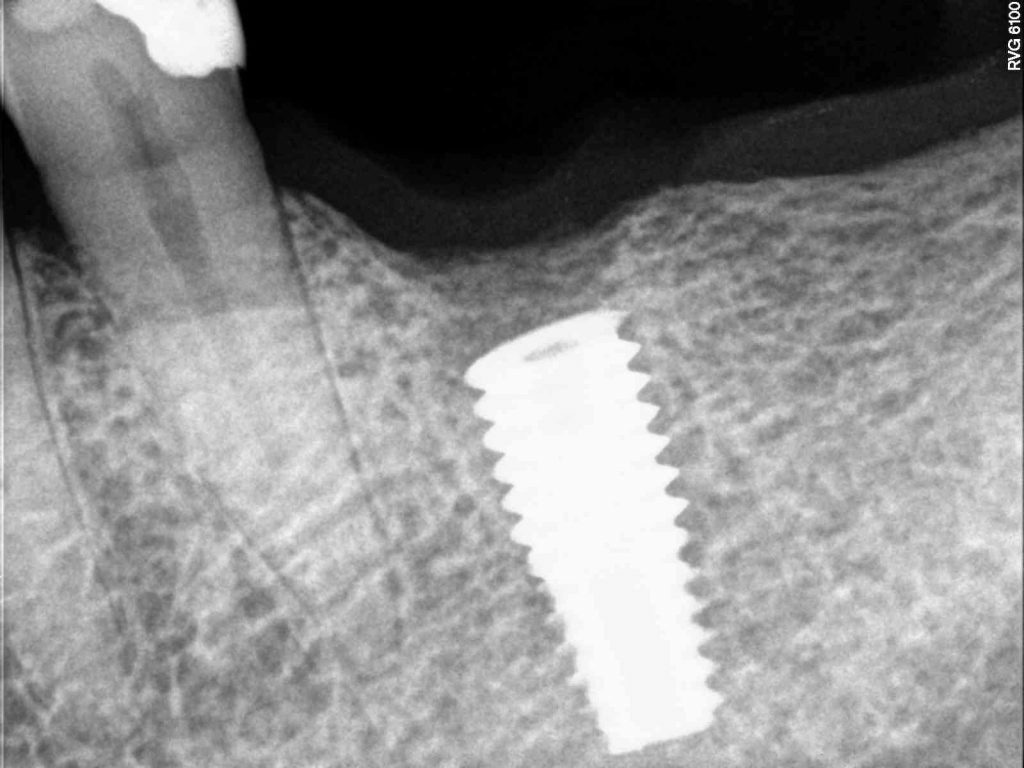
- Removal of implant using reverse torque explantation technique: If the implant fracture is relatively superficial and there is 3-4 mm of internal access hole remaining, then a reverse torque explantation technique may be effective in its removal. This is the most preferred and atraumatic approach in implant removal. A bone graft may be necessary after implant removal to restore bone for future implant placement.
- Removal of implant using bone trough technique: If the implant fracture is deeper and the reverse torque explantation device can not be engaged in the implant’s internal mechanism, then removal can be achieved by cutting a 0.5-1 mm of bone around the implant using a trough bur and then dislodging the fractured segment out of the bone. A more significant bone graft is often necessary to restore the bone for future implant replacement.
- Leave fractured implant in bone: If no implant replacement is planned in the same site, then one option can be to leave the fractured segment in the bone and allow the bone to heal over it. Leaving segment of dental implant in bone generally does not cause any problems.
How to minimize risk of dental implant fracture:
- Select widest implant possible for the tooth to be replaced. For molars, A minimum 6-mm wide implant is recommended. For premolars, 4- or 5-mm diameter is appropriate.
- Place more implants in the back (posterior) particularly in patients with higher biting force. More implants allow better distribution of occlusal (bite) load and hence are more protective under excessive forces. If you have missing molars, then replacement of both first and second molars with two implants are recommended.
- Minimize occlusal table size of the restoration: This refers to the actual width of the implant crown. The larger the crown, the more possibility for cantilever forces and hence increased risk of fracture. If larger crowns are necessary, then a wider dental implant should be selected to match.
- Avoid cantilever bridges: This is the situation when two crowns are placed on one implant. While this can be an effective design in the front, it is very risky in the back area of the mouth and should be avoided.
- Equilibrate the restorations: The implant restorations must be carefully checked for contacts under function and adjusted to remove any interference or lateral contacts that are not biologically compatible.
With proper treatment planning, selection of right implants, design of the restorations, and a thorough evaluation of the patient’s function and occlusal load, implant fractures can be prevented.
Dr. H. Ryan Kazemi is a board-certified oral and maxillofacial surgeon in Bethesda, MD